Trigeminal Neuralgia
Trigeminal Neuralgia
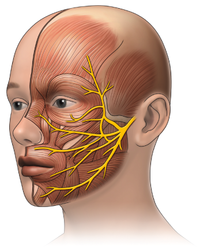 |
| trigeminal nerve(CN V) branching |
Trigeminal neuralgia (TN) is also called tic douloureux. The first account of TN is found in the writing of Avicenna in the 11th century, but it was John Fothergill who gave the modern description of TN in his 1773 paper on the subject . In the 21st century medicine, the pathophysiology of TN has been established through a deeper understanding of the physiology and development of imaging techniques. Due to its episodic nature, its initial presentation and the long-term management of these patients fall under the care of the general practitioners (GPs).
Prevalence
A survey of the GPs in the United Kingdom reported the incidence of TN as 26 per 100,000 per year, between 1992 to 2002 . The National Institute of Neurological Disorders and Stroke estimates the incidence rate of 12 per 100,000 people per year . There is gender variability in the incidence of TN with a female to male ratio of 1.74:1 with most of the cases occurring after 50 years of age .
Presentation
Almost 87% of all facial pains are related to dental or oral mucosal lesions .
clinical history, examination, investigations, and imaging are important to make a correct diagnosis . TN is characterized by an abrupt onset and short-lived unilateral shock-like pain, limited to the distribution of the trigeminal nerve. Triggers for classical TN (CTN) usually include mastication (73%), touch (69%), tooth brushing (66%), eating (59%), talking (58%), and cold wind on the face (50%). Combing hair is not usually a common trigger for TN. There can be concomitant background pain within the distribution of the nerve. Trigger zones are present in more than 90% of the patients, with touch and vibrations being the most common stimuli in provoking pain. Pain is usually distributed along the V2 and V3 branches
clinical history, examination, investigations, and imaging are important to make a correct diagnosis . TN is characterized by an abrupt onset and short-lived unilateral shock-like pain, limited to the distribution of the trigeminal nerve. Triggers for classical TN (CTN) usually include mastication (73%), touch (69%), tooth brushing (66%), eating (59%), talking (58%), and cold wind on the face (50%). Combing hair is not usually a common trigger for TN. There can be concomitant background pain within the distribution of the nerve. Trigger zones are present in more than 90% of the patients, with touch and vibrations being the most common stimuli in provoking pain. Pain is usually distributed along the V2 and V3 branches
Clinicians should be aware of other disorders such as painful trigeminal neuropathy that can present like TN. Herpes Zoster infestation of the trigeminal ganglion of the ophthalmic nerve, chronic paroxysmal hemicrania, Tolosa-Hunt syndrome, migraine, cluster headache, and glossopharyngeal neuralgia are among the differential diagnoses of TN.
Etiology and pathophysiology
Several observations lead to the vascular-compression theory of CTN, which indicates that TN is caused by the pressure of blood vessels on the trigeminal nerve as it exits the brain stem. Most commonly, a rostroventral superior cerebellar artery loop compresses the trigeminal nerve and causes the symptoms .
 |
| trigger points along facial areas of CN V |
Diagnosis
CTN is a clinical diagnosis based on the history of the patient and a thorough physical exam, particularly a neurological exam. Magnetic resonance imagining/angiography (MRI/MRA) is often used to confirm the diagnosis and to exclude other possible causes of facial pain. Imaging techniques can help locate the area of the neurovascular loop as well as find any secondary causes. Neurophysiological recording of trigeminal brainstem reflexes and trigeminal evoked potentials help detect the lesion . Medical treatment for most patients with CTN is required. Medical therapy helps provide relief from excruciating pain and decrease in pain frequency and duration as well as the associated symptoms. Patients who are resistant to or unable to tolerate medications can be candidates for surgical treatment.
Treatment
The European Federation of Neurological Societies and the Quality Standards Subcommittee of the American Academy of Neurology consider carbamazepine (CBZ) as the drug of choice for the treatment of TN.
CBZ is also the only Food and Drug Administration (FDA)-approved medication for the treatment of TN. CBZ is an anticonvulsant that is structurally close to tricyclic compound imipramine. It works by the inhibition of sodium channel activity and the modulation of calcium channels. Its efficacy in the treatment of TN is well established. In a review of several studies, CBZ provided a high level of pain control (58% to 100%), while the placebo success rate was only 0% to 40% . However, providers should be aware of tachyphylaxis with the use of CBZ. The typical starting dose is 100 to 200 mg twice daily and then is gradually increased to 200 mg. The usual maintenance dose is 600 to 1200 mg in divided doses with a desired therapeutic blood level of 4 to 12 ug/ml. The initial half-life of CBZ is around 30 hours, but because of auto-induction of cytochrome P450 isoenzyme CYP3A4, it is reduced to 10 to 12 hours. This decrease in half-life necessitates monitoring the serum levels, twice daily dose scheduling, or use of a time-release formulary. The presence of the human leukocyte antigen (HLA)-B*15:02 allele is a genetic susceptibility marker of developing Stevens-Johnson syndrome in high-risk (Asians) populations. Patients with Asian ancestry should be screened for this allele before starting CBZ, and if positive, the use of CBZ should be avoided. More common side effects include drowsiness, dizziness, and nausea. Severe side effects include aplastic anemia, hyponatremia, and abnormal liver function tests. Regular monitoring of blood counts, liver function tests, and serum sodium levels is recommended
CBZ is also the only Food and Drug Administration (FDA)-approved medication for the treatment of TN. CBZ is an anticonvulsant that is structurally close to tricyclic compound imipramine. It works by the inhibition of sodium channel activity and the modulation of calcium channels. Its efficacy in the treatment of TN is well established. In a review of several studies, CBZ provided a high level of pain control (58% to 100%), while the placebo success rate was only 0% to 40% . However, providers should be aware of tachyphylaxis with the use of CBZ. The typical starting dose is 100 to 200 mg twice daily and then is gradually increased to 200 mg. The usual maintenance dose is 600 to 1200 mg in divided doses with a desired therapeutic blood level of 4 to 12 ug/ml. The initial half-life of CBZ is around 30 hours, but because of auto-induction of cytochrome P450 isoenzyme CYP3A4, it is reduced to 10 to 12 hours. This decrease in half-life necessitates monitoring the serum levels, twice daily dose scheduling, or use of a time-release formulary. The presence of the human leukocyte antigen (HLA)-B*15:02 allele is a genetic susceptibility marker of developing Stevens-Johnson syndrome in high-risk (Asians) populations. Patients with Asian ancestry should be screened for this allele before starting CBZ, and if positive, the use of CBZ should be avoided. More common side effects include drowsiness, dizziness, and nausea. Severe side effects include aplastic anemia, hyponatremia, and abnormal liver function tests. Regular monitoring of blood counts, liver function tests, and serum sodium levels is recommended
Local anesthetics such as alcohol, glycerol, phenol, tetracaine, or bupivacaine injections are used in the diagnosis and treatment of TN . These percutaneous injections can provide relief from pain for a few months to years. Injections of botulin toxin A also help reduce the pain intensity and frequency in TN . Patients, whose symptoms are refractory to medical treatment or if they are unable to tolerate it due to side effects, are preferred candidates for surgical procedures for the treatment of TN. Usually, surgical therapies involve decompression of the nerve by resetting the vascular loop around the nerve or sometimes resetting the nerve that carries the pain signals
surgical treatment Percutaneous trigeminal ganglion balloon compression rhizotomy is usually reserved for patients who cannot tolerate the above-mentioned treatments or are refractory to it
Percutaneous radiofrequency gangliolysis, trigeminal ganglion compression, and retrogasserian glycerol rhizolysis are different techniques utilized to ablate the ganglion. These procedures have high initial success rates. Microvascular decompression (MVD) is conducted under general anesthesia using a microscope to identify the trigeminal nerves
other invasive procedure are described in other topics ...
surgical treatment Percutaneous trigeminal ganglion balloon compression rhizotomy is usually reserved for patients who cannot tolerate the above-mentioned treatments or are refractory to it
Percutaneous radiofrequency gangliolysis, trigeminal ganglion compression, and retrogasserian glycerol rhizolysis are different techniques utilized to ablate the ganglion. These procedures have high initial success rates. Microvascular decompression (MVD) is conducted under general anesthesia using a microscope to identify the trigeminal nerves
other invasive procedure are described in other topics ...
 |
| Diagnosis of dental and orofacial pain |
Related topics :












read alot to surpass boring 😉
ReplyDeleteThanks for taking the time to share this wonderful post with us. This was such an amazing article filled with so much informative information. Have a great rest of your day.
ReplyDeleteDentist Philadelphia
This is a knowledgeable blog and the information is very useful for me. I think all the interested people love to read this blog because this is the really good and knowledgeable blog.Trigeminal Neuralgia Treatment In Jaipur
ReplyDeleteHey thегe and Thank you so much for sharing this information. It has very useful. Please keep sharing.If you want more about the best treatment for .Trigeminal Neuralgia Treatment Kindly click the link
ReplyDeleteFacial Nerve Pain Relief in Coimbatore